Tuesday, December 31, 2019
Medical News Today: Researchers discover new autoinflammatory condition
Medical News Today: Unhealthful diet linked with vision loss later in life
Getting sleep in the hospital
If you or any of your loved ones has ever been hospitalized, one of the complaints you may have heard about most is how hard it is to sleep in the hospital. There are lots of things about hospital routines that can make things difficult for patients to sleep, besides noise and illness. While some hospitals have taken steps to ensure that patients are not interrupted unnecessarily at night, this is not universal. Here are some things you can expect, and some steps you might be able to take to help the hospital give you a better night’s rest.
Some reasons you might be woken at night might be unavoidable
You might be on a particular medication, such as certain antibiotics, that must be given in the middle of the night, depending on when the first dose was given, and blood tests for levels of some antibiotics must be timed to their dosing, resulting in blood draws in the middle of the night, too. If you are admitted to check for a heart attack, you might also be ordered for timed blood tests that might involve having your blood drawn in the middle of the night. Vital signs, such as pulse and blood pressure, are required to be taken every four hours for some conditions, which would also awaken you.
One study shows the top thing keeping patients awake is pain, followed by vital signs and tests, noise, and medications. Studies have also shown that hospital routines can disrupt patient sleep, and having a designated quiet time, where nonessential tasks are minimized and lights and noise are lowered, may help. Here is a partial list of things that keep patients awake, and what you might be able to do about them.
Pain. Pain is easier to control before it gets bad. Don’t hesitate to ask for pain medicine at bedtime, even if your pain is not yet severe.
You are woken up to have your blood pressure taken. Vital signs are usually taken every eight hours. Often these are done between 11 pm and midnight, after the night shift starts, but it’s often just after you have fallen sleep. Alternatively, the night shift could be taking your vital signs at 6 am, when you’d be awoken for other hospital routines anyway. If you are given the opportunity to give feedback during or after your stay, it would be important to mention this — hospital administrators look closely at patient feedback.
The IV pump that keeps beeping. This is usually because the flow of IV fluid is blocked (occluded), most often because the IV was inserted in the crook of your elbow. Thus, every time you bend your arm, the pump will alarm and start beeping. If this is the case, ask to have the IV put in a different place, like your hand.
You are woken to be given medications. Sometimes a medication or breathing treatment might be ordered “every four hours” or “every six hours” which means the nurse or respiratory therapist is required to wake you to give it to you even if you are asleep. You can ask if the order can be changed to four times a day instead of every six hours, or “every four hours while awake” so you don’t have to be woken.
Noise. Lots of things can be noisy in the hospital at night — staff voices, cleaning machines, your roommate if you have one. You can always ask to have your door closed, and you can ask someone to bring in ear plugs.
You are up all night urinating. If this is not the case when you are at home, it might be because you were ordered for a diuretic to be given late in the day, after 6 pm or so, or you are ordered for IV fluids at a rate that is higher than you actually require. Your nurse can ask the doctor to change these orders.
Blood transfusions at night. If you need a blood transfusion, it is best not to do it during sleeping hours, because it requires the nurse to monitor your vital signs frequently and would keep you awake for hours. If you need a transfusion at that hour, ask if it can possibly wait until daytime.
Frequent nighttime disruptions can often cause patients to want to nap during the day, and throw off their sleep schedules. Patients might already be weak and tired from their underlying illness. If you’re hospitalized, it’s important to keep your normal sleep schedule and circadian rhythm. During the day, keep the window shades open for natural light and keep the room dark during sleeping hours. An eye mask might be helpful if exposure to light at night is unavoidable. A favorite blanket, pillow, photos, and your favorite music can help you relax and be more comfortable.
My colleagues and I at Somerville Hospital (since closed to inpatients) found that when we instituted a program to decrease disruptions during the night, such as purposely avoiding all the things described above, patients used as-needed sedatives about half as often in the hospital. Most hospitals can do better to make nighttime routines friendlier for patients, but institutional change can be challenging. Knowing what to ask for is useful and will help move healthcare forward.
The post Getting sleep in the hospital appeared first on Harvard Health Blog.
Monday, December 30, 2019
Medical News Today: Could MDMA help treat mental health conditions?
Medical News Today: Should we all be eating more protein?
An omnivore’s dilemma: How much red meat is too much?
In October 2019, the Annals of Internal Medicine published controversial guidelines advising Americans to carry on consuming red and processed meat at current amounts. The guideline authors characterized meat-eaters as somewhat incapable of dietary change, and portrayed the benefits for reducing red and processed meat intake as insignificant. These guidelines contradict previous studies that link processed meat and red meat with early death and an increased risk of disease, including cardiovascular disease (CVD) and cancer.
If omnivores are confused, it’s hard to blame them.
Americans are eating less meat, but not less processed meat
To frame their argument, the article authors referenced an average meat intake from North America and Western Europe of two to four servings per week. But we are not France, and about a third of Americans eat more than this. In fact, on average we eat about five servings (17 ounces) of red and processed meat per week.
We have made progress decreasing our consumption of unprocessed beef, pork, and lamb over the past two decades. But our intake of processed meat remains unchanged: sausage, hot dogs, and ham reign among the nation’s most beloved processed meats.
Red meat and processed meat increase disease risk
The message from the Annals guidelines was perplexing and, at times, poorly translated by the media, with some headlines goading Americans to go full speed ahead on their intake.
This is particularly alarming, because recent research indicates eating 3 1/2 more servings of meat per week is associated with a higher risk of death. Consuming more than three additional servings may sound like a significant escalation. But consider that a standard serving equals about 3 ounces, a portion the size of a deck of cards. Eating a steakhouse filet, which typically weighs up to 12 ounces, you could consume roughly 3 1/2 servings in a single meal.
The connection is stronger for processed meats, which have a smaller standard serving size. For bacon lovers, eating a mere four slices more of thick-cut bacon a week is enough to increase risk of death.
Red and processed meat have also been associated with an increased risk of cancer. According to the World Health Organization’s International Agency for Research on Cancer, there is sufficient evidence to label processed meat as a carcinogen (a cancer-causing substance). Consuming a daily portion of less than two ounces per day — the equivalent of two slices of ham or bologna — is associated with increased cancer risk.
Eating less red meat makes room for healthier foods
Unfortunately, outlining the health hazards of red and processed meat sends a negative message and misses the bigger picture: many of us simply do not eat enough protective foods, and eating less meat would allow space for the foods we are neglecting.
According to the USDA, close to 90% of Americans do not eat the recommended amount of vegetables per day. (Most people should aim for two to four cups daily depending on their age and sex.) . Adults are not eating enough legumes, like beans and lentils, nor are we consuming enough seafood. The good news is that replacing some red and processed meat with whole grains, vegetables, and marine and plant-based proteins may help you live longer.
This is helpful for our collective health too, as livestock are responsible for 14% of greenhouse gas emissions that contribute to climate change and threaten our planet. (Seafood practices also contribute to global warming, but only lobster and crab come close to cattle, our country’s most popular red meat and the animal responsible for the greatest greenhouse gas emissions.)
Shift focus to the foods you should eat more of
Ultimately, we do Americans a disservice if we cast them as incapable of making change. We can’t assume that it would be a burden to switch from beef jerky to nuts or from ham to tuna.
But asking how much meat is too much is, perhaps, the wrong question. Rather, we should really be asking: what do we need to eat more of instead?
The post An omnivore’s dilemma: How much red meat is too much? appeared first on Harvard Health Blog.
Sunday, December 29, 2019
Medical News Today: Cholesterol levels in young adults can predict heart disease risk
Medical News Today: Mindfulness training may lower blood pressure
Saturday, December 28, 2019
Medical News Today: Intermittent fasting can help ease metabolic syndrome
Medical News Today: Passing kidney stones: 2-drug combo may relieve pain
Friday, December 27, 2019
Medical News Today: A key area of the brain is smaller in women on the pill
Medical News Today: High blood pressure research: 2019 overview
Should you use probiotics for your vagina?
You know probiotics can be good for your gut, but does your vagina need one too? You might think so, based on probiotic marketing these days. Probiotics are in everything from drinks to pills and powders, and in many cases, are being promoted as a means of improving your vaginal health.
Women seem to be listening, says Dr. Caroline Mitchell, assistant professor of obstetrics, gynecology, and reproductive biology at Harvard Medical School. Vaginal probiotic supplements are hugely popular. This includes both probiotic pills and suppository capsules that are inserted into the vagina using an applicator.
But evidence of effectiveness is scant. “There is almost no evidence that these have benefit for vaginal health. The studies are mostly poorly done and don’t adhere to rigorous reporting standards, even if they are randomized trials,” says Dr. Mitchell. But that hasn’t stopped companies from promoting products for that purpose.
However, while today’s vaginal probiotic products should be viewed with a healthy dose of skepticism, that may change as scientific knowledge builds. Meanwhile, here’s what’s known — and unknown — about probiotics and your vaginal health.
Sorting facts about probiotics from fiction
Vaginal probiotics are touted as a way to introduce live microorganisms into your vagina to improve health. It’s true that your vagina, like your digestive tract, is teeming with beneficial bacteria and other microorganisms. When it comes to vaginal health, some common gynecological conditions are thought to be caused by an imbalance of bacteria inside the vagina. More often than not, when women seek out probiotics, they’re doing it in an attempt to ease discomfort caused by two of them: bacterial vaginosis and yeast infection, says Dr. Mitchell.
Bacterial vaginosis is the most common vaginal infection in women of childbearing age. There’s still a lot that experts don’t understand about the condition, but it is associated with an overgrowth of harmful microorganisms (such as Gardnerella vaginalis or Prevotella), which outnumber healthier types of vaginal bacteria, including a common organism called Lactobacillus.
Vaginal yeast infection also stems from an imbalance in the vagina. But in this condition, the problem is a fungus called Candida, which overcomes healthy bacteria. Candida can exist normally in the vagina without any problem, but may cause trouble if it outnumbers other microorganisms.
“There are some women who could benefit from probiotics — at least in theory,” says Dr. Mitchell. Among them are women with bacterial vaginosis or yeast infection. For example, when it comes to recurrent bacterial vaginosis, the thinking is that introducing more of the helpful lactobacilli might protect against that overgrowth of harmful organisms, and consequently reduce recurrent infections. However, proof is lacking, says Dr. Mitchell. If that theory is shown to be true, a probiotic could be beneficial, but no one is sure. And it’s not at all clear that taking a probiotic orally will help the vagina.
There are also unknowns related to vaginal yeast infection. “In the vagina, yeast and lactobacilli coexist quite happily, while in the laboratory, lactobacilli can kill yeast,” says Dr. Mitchell. So, taking probiotics isn’t a scientifically based strategy, because real-life circumstances don’t match what happens in the laboratory.
For now, the only proven treatments for bacterial vaginosis and yeast infection are antibiotic or antifungal treatments, says Dr. Mitchell.
A solution springs from frustration
But sometimes women don’t respond to the standard treatments and experience recurrent problems that leave them searching for solutions. Dr. Mitchell says that some women she’s encountered are trying not only probiotic supplements, but also alternative treatments they’ve found on the Internet. These include putting yogurt-soaked tampons, tea tree oil, and even garlic cloves into their vaginas in an effort to introduce beneficial bacteria. These solutions, she says, are not only ineffective but highly inadvisable.
“It’s true that a compound in garlic, allicin, has been shown to kill yeast in a laboratory. But you cannot put enough cloves of garlic in your vagina — or take enough oral garlic capsules — to achieve the same effect,” says Dr. Mitchell. Tea tree oil also has no demonstrated benefit and can cause irritation. Yogurt-infused tampons don’t work either. Many probiotic supplements and most yogurts do contain Lactobacillus bacteria, but it’s generally not the same type of Lactobacillus found in your vagina. L. crispatus and L. iners are the most common species found in the vagina. Most probiotics and yogurt contain other species, such as L. rhamnosusor L. acidophilus, which are more common in the gut.
Benefit or harm?
There also isn’t enough information to determine if introducing new bacteria using probiotics might do more harm than good. One study published in September 2018 in the journal Cell found that when people were given a probiotic after antibiotic treatment, their natural gut bacteria actually took longer to recover than did the gut bacteria of people who didn’t take the probiotic.
What I tell people is that over all, vaginal probiotics are probably a waste of money,” says Dr. Mitchell. “But if you are going to pick one and you really want to try one, the probiotics that seem to show some benefit in studies are ones containing Lactobacillus rhamnosus GR-1.”
Keep in mind that supplements, unlike medications, are not FDA-regulated. “Studies have shown that when these products are cultured, they often don’t have as much of what is on the label as promised, or don’t even contain what is on the label,” says Dr. Mitchell. The FDA has also found that some supplements contain potentially dangerous contaminants.
The post Should you use probiotics for your vagina? appeared first on Harvard Health Blog.
Thursday, December 26, 2019
Medical News Today: How do fruit and veg reduce colorectal cancer risk?
Medical News Today: Ultrasound with MRI improves prostate treatment
Eosinophilic esophagitis: A new food-related allergic condition on the rise?
In the early 1990s, doctors began describing a new condition affecting the esophagus of patients who were predisposed to allergies including food allergy, asthma, and eczema, and who were having trouble swallowing. Today, we call this condition eosinophilic esophagitis (EoE).
What is EoE?
EoE is an allergic inflammation of the esophagus that causes a range of symptoms. Adolescents and adults most often experience it as difficulty swallowing, sometimes feeling like food moves too slowly through the esophagus and into the stomach. In some cases, food actually gets stuck (and may require urgent removal). Children and some adults primarily experience reflux symptoms and abdominal pain rather than difficulty swallowing.
In most cases, EoE develops as an allergic response to certain foods including wheat, milk, egg, soy, nuts, and seafood. If it is not properly diagnosed and treated, EoE may lead to permanent scarring or strictures (narrowing of the esophagus).
How is EoE diagnosed?
When EoE is suspected, generally the first test is an upper endoscopy, in which a flexible tube with a small camera and a light on one end is used examine the esophagus. The endoscopy usually reveals characteristic features of EoE, such as concentric rings and linear furrows or vertical lines, as well as small white spots or plaques.
The diagnosis is confirmed if biopsies from the esophagus reveal the hallmark increase in eosinophils. Eosinophils are a relatively rare type of immune cell that play a prominent role in allergic disorders including EoE and asthma.
How common is EoE?
EoE can affect both men and woman of any age, but it appears to be most common in men in their 30s and 40s. It is currently estimated that EoE may affect up to one in 2,000 adults in the US, and evidence suggests that the numbers have been growing. A recent review of nearly 30 studies in Europe and North America found that there has been a progressive increase in the number of new EoE cases, especially since the early 2000s.
The rise in EoE cases may be partly due to greater awareness of the condition and more widespread use of endoscopy. But a number of studies have confirmed a true rise in the incidence of the disease.
Why might EoE be on the rise?
The exact reasons for the rise of EoE are unknown, and it is especially puzzling that in many cases EoE results from an allergic sensitivity to a food that has been well tolerated up to that point.
There are several hypotheses about why EoE is increasing. Many of them relate back to the idea that EoE, and other allergic and autoimmune diseases, seem to correlate with decreased exposure to microbes and infections. Possible explanations that have been explored include:
- The hygiene hypothesis: do fewer childhood infections equal more allergic diseases?
- Microbial dysbiosis: has the modern/Western diet and lifestyle changed our microbiome?
- Environmental factors: might changes in food production, genetic modification of crops, chemical additives, food processing, and pollutants play a role?
- Declining frequency of H. pylori infection: might this common stomach bacteria (a common cause of peptic ulcers) be protective against some allergic diseases?
- Increasing frequency of gastroesophageal reflux disease (GERD): could acid reflux break the barrier of the esophagus and allow food allergens to stimulate the immune system?
- Increasing use of acid-suppressing medications: does the use of antacids, especially early in life, change the microbes in the esophagus or somehow otherwise alter the risk of later food allergy?
How is EoE treated?
There are currently no FDA-approved treatments for EoE. Most people are initially treated with a proton-pump inhibitor (PPI) antacid, which resolves EoE in up to half of cases. If this does not work, either a mild topical steroid or identification and elimination of specific dietary triggers is attempted.
When steroids are used to treat EoE, these are generally in a liquid formulation that is swallowed, rather than inhaled as they would be for asthma. Swallowed steroids act locally on the esophagus and are minimally absorbed through the gastrointestinal tract. Although steroids for EoE are generally safe and effective, they do not lead to a long-term cure because the disease tends to come back as long as patients continue to eat foods that trigger the underlying allergic response.
Patients may also opt to identify their food trigger and eliminate it from the diet, and this represents a more definitive treatment approach. Unfortunately, currently available allergy testing does not accurately predict the foods that cause EoE. Trigger foods generally need to be identified using a process of food elimination and reintroduction. Wheat and dairy are the two most common triggers for EoE, and patients will often start by eliminating these two foods for about eight weeks. At that point, their symptoms are reassessed, and they also undergo a repeat endoscopy with biopsies to determine if the eosinophils have disappeared in response to the dietary changes.
Several medication therapies are on the horizon. These include better formulations of steroids and biologic medications that reduce the activity of eosinophils.
Summary
If you are having trouble swallowing or have experienced episodes of food getting stuck in the esophagus, particularly if you have other allergic conditions, discuss your symptoms with your doctor. Unrecognized or untreated EoE can lead to permanent damage to your esophagus.
For more information or to learn about strategies for living with EoE, visit the American Partnership for Eosinophilic Disorders.
The post Eosinophilic esophagitis: A new food-related allergic condition on the rise? appeared first on Harvard Health Blog.
Wednesday, December 25, 2019
Medical News Today: What causes uncontrolled laughter in epilepsy?
Medical News Today: How to stay healthy on Christmas Day
Tuesday, December 24, 2019
Medical News Today: For rats, empathy may be a survival strategy
Medical News Today: Aspirin: Friend or foe after breast cancer?
Medical News Today: A guide to the best probiotics
Medical News Today: What is the link between depression and anxiety?
Medical News Today: What to know about fever during pregnancy
Medical News Today: Everything you need to know about trigger point injections
How to help your baby through shots and blood tests
As much as we try to avoid having our babies go through pain, sometimes it is inevitable — and sometimes, as is the case with vaccinations and blood tests, pain is part of something that is ultimately important for the baby’s health and well-being.
Luckily, shots and blood tests are both quick. But there are things you can do to help your baby feel less pain, be less afraid, and get through the procedure more easily.
Helping your baby through the pain of shots and blood tests
Here are some suggestions that will help:
- Hold your baby. Having you be close by, and feeling your skin against theirs, can be very comforting.
- Swaddle your baby. When babies are wrapped up tightly, it helps them contain their bodies and their emotions. Obviously, shots and blood tests involve at least one leg or arm, so you can’t completely swaddle them, but you can swaddle whatever isn’t in use.
- Breastfeed, if possible. It’s not always possible for the nurse or the person drawing blood to do their job while the mother nurses because it can be hard to hold the child still, and sometimes people worry about the baby choking on milk when he or she cries. But if it is possible, it can be helpful.
- Use a pacifier. Sucking often soothes babies.
- Talk to your baby. Hearing your voice is both calming and distracting to babies.
- Talk to your doctor about using sugar water. Studies have shown that dipping a pacifier in sugar water or putting some into the baby’s mouth with a syringe can make a procedure less painful. It’s not fully clear how it works; it may activate the body’s natural systems for fighting pain.
As soon as the shot or blood test is done, pick your baby up and hold him or her close. That way the baby knows that it’s all over — and that you are there to take care of them.
Most of the time, babies are fine once the worst of it is over. But sometimes babies can have soreness where the needle went in, and it’s not uncommon for babies to feel uncomfortable or a bit sick for a day or so after vaccines. All the suggestions above can help with lingering discomfort. Usually medication isn’t needed, and after immunizations, using medications like acetaminophen can sometimes decrease the effectiveness of the vaccine itself.
Your doctor can help you decide what makes sense for your baby and your situation.
Follow me on Twitter @DrClaire
The post How to help your baby through shots and blood tests appeared first on Harvard Health Blog.
Monday, December 23, 2019
Medical News Today: Home remedies for premature ejaculation
Medical News Today: Can the keto diet treat epilepsy?
Medical News Today: What to know about peeing after sex
Medical News Today: What are the differences between cage-free, free-range, and pasture-raised eggs?
Medical News Today: Everything you need to know about microneedling with PRP
Medical News Today: Causes of heavy vaginal discharge
Medical News Today: Letter from the Editor: Time to reflect
Medical News Today: Why is it so difficult to say no to that piece of cake?
Medical News Today: Infections: How do our bodies know when to retaliate?
A new look at steroid injections for knee and hip osteoarthritis
Osteoarthritis is a common and potentially debilitating condition. It’s a degenerative joint disease (often called the “wear-and-tear” type) in which the smooth lining of cartilage becomes thinned and uneven, exposing the bone beneath.
Although osteoarthritis is tightly linked with aging, we now know there is more to it than age alone: genetics, weight, physical activity, and a number of other factors can conspire to make it more likely that someone will develop osteoarthritis while someone else won’t. Osteoarthritis is the primary reason that more than a million joints (mostly hips and knees) are replaced each year in the US.
Treatments short of surgery can help but they don’t always work well, don’t cure the condition, and may be accompanied by side effects. Surgery is usually the last resort, reserved for people who have declining function, unrelenting pain, or both despite trying other treatments such as pain relieving, nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, others) or naproxen (Aleve, others), or injections of steroids or hyaluronic acid (a type of lubricant). Nonmedication approaches can also help, such as loss of excess weight, physical therapy, or use of a cane or brace.
Calling steroid injections into question
Steroid injections can quickly relieve inflammation in the joints, and the effects may last from several weeks to several months. I’ve seen a number of patients who got significant relief from steroid injections every three or four months. But, a new report of one medical center’s experience and a review of past research came to some concerning conclusions about joint injections for osteoarthritis of the hip or knee. These included:
- a lack of compelling evidence that they work
- about 7% to 8% of people getting steroid injections seem to worsen, with their arthritis accelerating “beyond the expected rate”
- unusual fractures may occur (in about 1% of people)
- bone damage (called osteonecrosis) (in about 1% of people).
Other side effects include a temporary increase in blood sugar, bleeding into the joint, and, quite rarely, infection. And, of course, the injection itself can be painful, although numbing medication is usually provided.
The authors suggest that doctors order x-rays before each injection and not perform injections if there is evidence of any of these complications or unexplained pain. However, it’s not clear how effective this approach would be.
Now what?
The findings of this report regarding injections of steroids for knee and hip osteoarthritis are disappointing, especially for those who have not improved with other treatments.
Regarding the benefit of the injections, it’s important to keep in mind that even if the average benefit of a treatment is small, it does not mean that treatment is useless. Though temporary, some people do report significant improvement with steroid injections.
It’s also not entirely clear that the problems described in this study are actually caused by the steroid injections. And, from my own experience, the rates of complications seem high to me. That said, a 2017 study did find that people getting steroid injections had more thinning of joint cartilage than those getting placebo injections.
In my own practice, I’ll still offer a steroid injection for osteoarthritis, but only after carefully reviewing the potential risks and benefits. If it is not terribly helpful, I would not encourage repeated injections. On the other hand, if it works well, a limited number of injections (up to three or four per year is a common limit) may reduce pain and improve function and quality of life.
Restricting the injections to those who improve the most and limiting the number of injections each year may be a better strategy than eliminating steroid injections altogether, especially since the most serious side effects are quite rare.
We’ll need additional studies that examine the type, dosage, and frequency of steroid injections that might provide more benefit than risk. And we’ll need better ways to predict who will improve the most. Until then, I think it’s important to keep an open mind about just how helpful — and how safe — steroid injections for osteoarthritis truly are.
Follow me on Twitter @RobShmerling
The post A new look at steroid injections for knee and hip osteoarthritis appeared first on Harvard Health Blog.
Sunday, December 22, 2019
Medical News Today: Finding life's meaning can keep us healthy as we age
Medical News Today: Dementia: Obesity, but not diet or inactivity, raises risk
Saturday, December 21, 2019
Medical News Today: Inflammatory marker could be early warning for dementia
Medical News Today: 2019 in medical research: What were the top findings?
Medical News Today: What causes arm numbness?
Medical News Today: What causes chest pain on the left side?
Medical News Today: What are the early signs of lung cancer?
Flu cases reported at increasing rate; 6 deaths in Ky. this season
In the week ended Dec. 14, there were two deaths, bringing the statewide total for the current flu season to six, according to the state Department for Public Health.
During that week, 814 new cases of the flu were reported. Five of the deaths were people 18 or older and one was under 18. Twelve of the state's 17 health regions reported increased flu activity during the week.
The federal Centers for Disease Control and Prevention estimates that the flu has killed between 12,000 and 61,000 people annually in the U.S. since 2010.
Gov. Beshear rescinds Bevin's Medicaid waiver plan but asks federal government to let Kentucky keep four parts of it
Kentucky Health News
As he promised in his campaign, Democratic Gov. Andy Beshear rescinded defeated Republican predecessor Matt Bevin's Medicaid plan, which included highly controversial work requirements. But Beshear said he also wants to keep using four parts of it.
 |
| Beshear signs executive order on Medicaid. (Melissa Patrick photo) |
"We were convinced that the only way to address this waiver initially was to fully rescind it and then move forward on addressing or creating those programs that might be beneficial inside of it," he said at a Dec. 16 news conference, where he signed an order rescinding Bevin's request for a waiver of federal rules to implement the plan.
The plan would have required "able-bodied" adults on Medicaid to work or participate in approved "community engagement" activities 80 hours a month and pay small, income-based premiums monthly to stay covered.
Bevin's original proposal projected that in five years the Medicaid rolls would have 95,000 fewer people with the plan than without it, largely because of non-compliance with its requirements, including monthly reporting.
"My faith teaches me that rescinding this waiver is not only the right thing to do, it is the moral, faith-driven thing to do," Beshear said. " I believe health care is a basic human right."
"That's spot on," said Ben Chandler, president and CEO of the Foundation for a Healthy Kentucky. "That's what I was always taught Jesus Christ was about, is about including people and giving them a hand up when and where you could. And that's what this is and I think it's a great thing."
Chandler noted that the foundation had committed to helping the state keep people from losing coverage under the waiver, and could now use those resources for other efforts.
"We had been concerned about the hundred thousand or so people who were predicted to ultimately lose their coverage had the waiver been implemented." Chandler told Kentucky Health News.
Bevin's proposal had already been struck down twice by a federal judge in Washington, D.C., and was awaiting the decision of an appeals court. Beshear told reporters that by ending the waiver, Kentucky would no longer be involved in that lawsuit. Arkansas, which implemented a similar plan before being sued, will remain in the suit.
Beshear's office hinted in a news release that he might use his order as partial grounds for also rescinding "the $8 billion in Medicaid managed care contracts that the previous administration awarded with just 11 days left in the administration. Those contracts were awarded based on the waiver." Legislators in both parties have objected to the awards.
Two days after signing the executive order, Beshear's administration sent a letter to the Centers for Medicaid & Medicare Services saying his request would not apply to four provisions in the waiver.
Two of those provisions involve substance use disorder. One allows non-emergency medical transportation for methadone treatment for most people on Medicaid; the other involves the substance-use disorder program that is available to all Kentucky Medicaid beneficiaries.
The third involves a provision that extends Medicaid coverage to former foster-care youth who were the responsibility of another state before moving into Kentucky; the fourth allows a family to coordinate its annual Medicaid re-determination with an open-enrollment period for an employer-sponsored insurance plan. It would include any children who are enrolled in Medicaid or in the Children's Health Insurance Program and are covered by a parent or caretaker's plan.
The judge's rulings against the waiver had no effect on those four elements, as the letter to CMS notes. It also points out that the four have operated without interruption in Kentucky during the suit.
"I am glad Governor Beshear sees the importance of keeping these positive policy changes," Marcie Timmerman, executive director for Mental Health America of Kentucky, told Kentucky Health News in an e-mail. "Mental health and substance use disorders affect people from every race, class, ethnicity, and orientation. The commitment of Kentucky to help our citizens have access to substance use disorder recovery is something we can all build on."
Kristen Arant of Newport, who receives coverage through expanded Medicaid, told reporters at the news conference that it had saved her life, allowing her to receive treatment for her substance-abuse disorder. She's now a college graduate and a social worker.
“Health care is not a luxury," she said. “It is not a commodity. It is a God-given right. People who do not feel well have the right to feel well. People who need medications have the right to have access to those medications."
The expansion has increased by more than a 500% the number in Medicaid beneficiaries receiving treatment for a substance-use disorder, said Emily Beauregard, director of Kentucky Voices for Health. She called Beshear's order a tremendous victory for the 16 plaintiffs who challenged Bevin's plan in federal lawsuits.
The Kentucky Equal Justice Center, which was largely behind the lawsuits that prevented the plan from going into effect, are "real heroes in this," Chandler said.
Center Director Richard Seckel diverted his appreciation to the 16 plaintiffs, calling them courageous. "We do hope that as this suit goes on with Arkansas that there will be findings that this waiver never should have been approved in the first place," he said.
Kentucky's Medicaid program covers about 1.3 million people; about 600,000 of them are children, and nearly 450,000 of the total are covered the expansion. Each month, tens of thousands of Kentuckians go on and off the program as they gain or lose eligibility.
"On any given day, most Kentuckians are simply a lost job, reduced work hours, a new baby, an accident or an illness away from qualifying for programs like Medicaid," Beauregard said. "That's why we call it a safety net."
Friday, December 20, 2019
Medical News Today: Liver function tests: What to know
Medical News Today: What to know about RSD
Medical News Today: What to know about the Moro reflex?
Medical News Today: What is the relationship between depression and sleep?
Medical News Today: Meningococcemia: Everything you need to know
Medical News Today: Vaping: Is it bad for you?
Medical News Today: Processed meat and cancer link depends on nitrite content
Medical News Today: Does your season of birth affect your mortality risk?
Medical News Today: Cardiovascular disease: Dietary cholesterol may not raise risk
Medical News Today: What to know about a CSF leak
Medical News Today: Is tonsillitis contagious?
Medical News Today: What to know about dysarthria
Researchers urge prostate cancer screening for men with BRCA gene defects
Prostate cancer screening with the prostate-specific antigen (PSA) test has been criticized for flagging too many slow-growing tumors that might never be life-threatening.
But some men have inherited gene defects that boost their risk of developing prostate cancers that can be quite aggressive. Is PSA screening particularly well-suited for these genetically defined groups? New research suggests the answer is yes.
In November, a team of British scientists released highly anticipated findings from a study of PSA screening in men with defects in a pair of important genes called BRCA1 and BRCA2. Better known for increasing the odds of breast and ovarian cancer in women, BRCA gene defects are also risk factors for aggressive prostate cancer in men. Cells with defective BRCA genes have a compromised ability to repair the DNA damage they sustain routinely every day. As that damage accumulates, those cells become prone to forming tumors.
What the investigators wanted to know was if PSA screens detect more prostate cancers in men who test positive for BRCA mutations than those who do not. To find out, they screened just over 2,900 men ages 45 to 69 who were split into four groups: a BRCA1 mutation-positive group, a BRCA2 mutation-positive group, and two groups that tested negative for mutations in either gene. The men were screened annually for four years, and had a prostate biopsy if their PSA levels ran higher than 3.0 nanograms per deciliter.
What the results show
In all 357 men were biopsied, and 112 of them were diagnosed prostate with cancer. The BRCA2 mutation carriers had the greatest cancer risk: 5.2% of them were diagnosed with the disease, and most of their tumors had intermediate- or high-risk features. BRCA1 mutation carriers had a lower risk: 3.4% of them were diagnosed with prostate cancer. And the men who tested negative for BRCA1 and BRCA2 mutations had the lowest risk overall, with diagnosis rates of 3.0% and 2.7% respectively.
Based on the results, Ros Eeles from the Institute of Cancer Research in London, who led the research, issued a statement calling on regulatory bodies to update guidance so that men with BRCA2 defects can get regular PSA screening after age 40.
Most expert groups in the United States recommend that doctors start talking about the pros and cons of PSA testing with patients who are 55 or older. However, guidelines are being rewritten to focus screening on high-risk groups at younger ages, and BRCA2 mutation carriers are widely considered to be in the highest-risk category.
Men should consider being tested for BRCA mutations under the following conditions:
- If there’s a history of prostate, breast, or ovarian cancer in the immediate family, particularly among younger members
- if other family members test positive for BRCA1 or BRCA2 mutations
- if they are of Ashkenazi Jewish descent, since BRCA mutations occur frequently in this ethnic population.
Dr. Marc Garnick, Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, and editor in chief of HarvardProstateKnowledge.org, says new guidelines that should be available soon will provide more information for families at risk of these cancers. If possible, he says, men should consider getting a PSA test when they’re 10 years younger than the age at which the youngest family member was diagnosed. Fortunately, he adds, new tailored treatments are becoming available for BRCA mutation carriers, and studies so far show promising responses.
The post Researchers urge prostate cancer screening for men with BRCA gene defects appeared first on Harvard Health Blog.
Wearables and sleep: What can they really tell us?
Smart devices are everywhere, including wrist-based monitors. These wearables promise to count our steps, remind us to move, and provide insight on our sleep. But can we trust them to measure our sleep accurately?
Most wrist-based devices are based on an accelerometer, which measures wrist movement. The data gathered from the accelerometer — how often the wrist moves and how forceful that movement is — are coded as sleep or wake. In some cases, programs will also label sleep as light or deep, seeming to imply that the sleep is good or bad. Some devices also monitor heart rate. Small variations in the timing of heart rate — which occur naturally under certain situations with a regular heart rhythm — may provide some clues about sleep stage as well. During stable deep sleep, breathing is typically very regular, and so is heart rate.
After these wrist devices collect data on our movements and/or heart rate during sleep, it is wirelessly transmitted to our phone or computer, and software programs analyze it to create charts and graphs that allow us to “see” our sleep.
Sleeping is believing, right?
It can be nearly magical to go to bed, sleep, and then instantly get a graph that shows what we did while we were sleeping. Was it a good night? How much deep sleep did we get? A few taps on the phone will show the truth. A graph will tell us how we spent the last several hours, with a breakdown of time awake, time in deep sleep, and light sleep. We may even get an overall “score” for the night. This is data-based, so it must be accurate, right? Turns out, the answer is much more uncertain.
How well do these devices measure sleep?
First, it is worth noting that the software algorithms that decide what is sleep and what is wake are a bit of a “black box.” These are proprietary, owned by the various companies that make the devices, meaning sleep doctors and researchers don’t know exactly how the programmers decided to make these determinations. Between different brands, or even different devices within a brand, the software code, and therefore sleep interpretation, could vary.
Consider that perhaps one wrist device determines that you’re awake after a bunch of forceful movements — think brushing your teeth — while for another device, a single small twitch of the arm may be considered being awake. How many movements mean we’ve woken up? One? Ten? Over what time period, one movement per minute? Ten movements over two minutes? How forceful do those movements have to be? How does the software decide we’re up for good or if we fall back asleep after movement? How good is the device at even catching movement — does it know if the wrist device is too loose? With all of these factors, the possibilities to code the data and interpret the data are infinite.
Second, there’s little to no data that compares wearable devices to research or clinical measurements. Actigraphs are small wrist-based devices that sleep providers and researchers utilize to measure sleep over longer periods. Similar to the consumer-available devices, they use accelerometers to sort sleep versus wake. Actigraphs, however, have been extensively studied and compared against sleep logs, sleep studies, and other data. Sleep providers have a fairly good sense of their strengths and limitations, and therefore how to use the data. The consumer devices are rapidly changing — newer monitors, frequent software upgrades. In general, the studies suggest that these wrist devices overestimate sleep duration (how long we’re asleep), and how much of the night is spent asleep (sleep efficiency).
Finally, there’s even less data on how these devices are impacted when there is a coexisting sleep or medical condition, or by medications. Consider a patient with insomnia who meditates when he can’t sleep and lies still in bed. This absence of movement and steady breathing could easily be misinterpreted as sleep by a wrist-based device.
What’s the gold standard for measuring sleep?
A sleep study, also called a polysomnography, measures brain waves, muscle tone, breathing, and heart rate, while a technician supervises, often in a hospital setting. The information from the brain waves determines wake versus sleep, and the stage of sleep. This is considered the gold standard for determining sleep characteristics in most circumstances. However, it is time- and labor-intensive, and expensive (and not always covered by health insurance).
Should we pay any attention to these devices?
Wrist-based devices seem to be here to stay, and people are going to be curious about their sleep. In general, I counsel my patients to review their sleep data with a grain of salt. It’s just one piece of the picture to incorporate, and doesn’t substitute for a quality sleep log or other forms of sleep assessments. The benefit is that the collection of this data is fairly passive, and can be done for longer stretches of time to gain insight into patterns.
Keeping in mind how these wearables measure sleep helps us know what they can and can’t do. In general, the devices probably do give us a rough sense of the time we’re spending in bed (which may or may not equal sleep time), and the regularity of sleep zone (the time we slept or tried to sleep between going to bed and getting up). Gaining insight on these two factors can be very helpful, and hard to pin down for some patients in other ways. Though the wrist devices don’t substitute for a medical opinion or sleep study in a hospital, if they help us reflect on our sleep and how much (or little) we’re getting, they may have a role if used carefully.
The post Wearables and sleep: What can they really tell us? appeared first on Harvard Health Blog.
Thursday, December 19, 2019
Medical News Today: What causes acid reflux and shortness of breath?
Medical News Today: Breast reduction surgery: Everything you need to know
Medical News Today: What to know about alcohol and the keto diet
Medical News Today: What to know about eco-anxiety
Medical News Today: Belly fat may reduce mental agility from midlife onward
Medical News Today: What causes cells to age?
Medical News Today: Ultra-processed foods may raise the risk of type 2 diabetes
Health officials warn outbreak of drug-resistant bacteria is likely coming from petting puppies in pet stores; 3 of 30 cases are in Ky.
Kentucky Health News
Getting a puppy for Christmas? Keep clean and take it to a vet. At least 30 people in 13 states have been sickened by a drug-resistant bacteria that federal health officials say was likely picked up from puppies in pet stores, three of them in Kentucky.
 |
| Getty Images photo, via WJW-TV, Fox 8 Cleveland |
The CDC noted that the hospitalized ranged in age from 8 months to 70 years old.
Among 24 people with infections who were interviewed, 21 said they had recently touched a puppy and 15 of those said they did so in a pet store. All of the cases were reported between January and November.
"Campylobacter bacteria can spread to people through contact with poop of infected animals and contaminated food or water," says the release.
Infection from the Campylobacter bacteria is one of the most common causes of diarrheal illness in the United States, infecting more than 1.5 million people every year, says the CDC. Most cases are not part of a recognized outbreak.
The release notes that a single, common supplier of puppies has not been identified. However, 12 of those who had contact with a puppy did so at a Petland store, and five of the 12 were Petland employees. Petland has two locations in Kentucky, in Florence and Ashland.
The CDC adds that the strain of Campylobacter in this outbreak appears to be related to a strain that caused a similar outbreak of puppy-related human illness in 2016.
In a statement, Petland said that just like a 2016 outbreak, this specific Campylobacter strain has not originated at any specific Petland store. The company said it implemented all recommended protocols from federal and state officials to prevent human and dog illness after that outbreak.
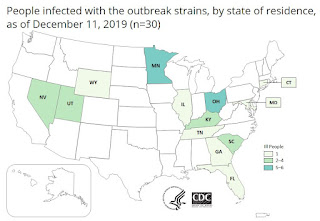 |
| Campylobacter jejuni oubreak as of Dec. 11, 2019 |
Illnesses have been reported in Connecticut, Florida, Georgia, Illinois, Kentucky, Maryland, Minnesota, Nevada, Ohio, South Carolina, Tennessee, Utah and Wyoming.
Symptoms of Campylobacter infection include diarrhea, fever and stomach cramps that begin two to five days after being exposed to the bacteria. The illness usually lasts about a week and most people recover without antibiotics. Antibiotics are needed for patients who are very ill or those with severely weakened immune systems.
The CDC encourages people to make sure they take a new puppy or dog to a veterinarian for a checkup within a few days after getting it because puppies and dogs can carry the Campylobacter germs even while appearing healthy and clean.
The agency also advises people to always wash their hands thoroughly with soap and water after touching a puppy or dog, after handling their food and after cleaning up after them. Also, don't let dogs lick around your mouth and face, open wounds, or areas with broken skin.
The release says the CDC the investigation is ongoing and the agency will provide updates when more information is available.
Bill to raise to 21 legal age to buy tobacco and e-cigarettes, pushed by McConnell and e-cig companies, awaits president's signature
Kentucky Health News
Legislation to raise the nationwide legal age to buy tobacco produces, including electronic cigarettes, from 18 to 21 passed Congress as part of the year-end spending bill and went to President Donald Trump for his expected signature. It passed the House Dec. 17 and the Senate Dec. 19.
“I’m proud the Senate approved legislation today including our Tobacco-Free Youth Act to help address this urgent crisis and keep these dangerous products away from our children," Senate Majority Leader Mitch McConnell, who engineered the move, said in a news release.
U.S. Sen. Tim Kaine, a Democrat from Virginia, who co-sponsored the measure, called its passage an "enormous victory for the health of our young people" and said in addition to reducing youth tobacco use, it would save 223,000 lives.
"This is one of many steps we should take to tackle the youth e-cigarette epidemic that touches every corner of our nation," Kaine said in a news release.
More than 6 million U.S. middle and high school students are current users of tobacco products, and 5.3 million of them, or 85 percent, are using e-cigarettes, according to the latest annual National Youth Tobacco Survey.
The latest data for e-cigarette use by Kentucky teens, from 2018, shows e-cig use had nearly doubled since 2016, with more than one in four high-school seniors and one out of seven eighth-graders reporting they used the devices, the Kentucky Incentives for Prevention study found.
“The dangers of nicotine on young people’s development—especially on their brains and lungs—can inflict life-long damage. Raising the minimum tobacco purchase age to 21 will help keep these harmful products away from our kids, and I can’t thank Senator McConnell enough for his vision and leadership for our children’s future," state Rep. Kim Moser, R-Taylor Mill, chair of the state House Health and Welfare Committee, said in McConnell's release.
In a separate release issued earlier this week, Ben Chandler, president and CEO of the Foundation for a Healthy Kentucky, praised McConnell's work. He added that the state legislature, which convenes Jan. 7, will need to change state law to comply with the federal statute. Sen. Ralph Alvarado, R-Winchester, has prefiled a bill to raise Kentucky's legal age to 21 from 18.
"This bill is a critical step toward reversing the skyrocketing rates of youth vaping nationwide and in Kentucky," Chandler said. "We encourage the Kentucky legislature to demonstrate similar leadership in passing Sen. Alvarado's Tobacco 21 bill quickly this coming year."
A similar bill was introduced in the last legislative session, but tobacco-friendly senators blocked it.
Terry Brooks, executive director of Kentucky Youth Advocates, also praised the legislation.
"Kentucky Youth Advocates thanks Leader McConnell for leading the way in Congress on this critical issue to help keep Kentucky kids—and kids across the nation—healthier and prevent life-long addiction to nicotine," Brooks said in a statement.
Already, 19 states have raised the tobacco age to 21, along with Washington, DC and over 530 localities, although the strength of their laws vary substantially, according to the Campaign for Tobacco-free Kids. E-cigarette companies see the law as a way to limit other forms of regulation aimed at limiting smoking and e-cig use by teenagers.
In the latest Kentucky Health Issues Poll, six in 10 Kentuckians said they would support increasing the minimum age to purchase tobacco products to 21, with majorities in each political party.
In addition to Alvarado's bill, Kentucky lawmakers have pre-filed several other bills to thwart the surge in teen use of e-cigs, including one to ban the sale of flavored e-cigs; one to impose registration and licensing requirements to sell them; and one to tax them at the same rate as traditional cigarettes.
A low-tech school vacation: Keeping kids busy and happy without screens
As we near the holiday season, along with trying to keep track of holiday events, parties, and gifts, parents have to think about what to do with their children during school vacation. Given how exhausting the holiday season can be, it’s understandable why parents often let their children spend hours with the TV, tablet, or video games. After all, happy, quiet kids make for happy parents who can finally get stuff done — or relax.
Except kids are spending way too much time in front of screens. According to Common Sense Media, kids ages 8 to 12 are spending nearly five hours a day on entertainment media — and tweens and teens are spending seven hours. This is just entertainment media; it does not include time spent using screens for school or homework.
Given how enticing entertainment media can be, those numbers can easily go higher during unscheduled times like weekends and school vacation. That’s why it’s good to be proactive and come up with other activities. Below are some ideas for parents and caregivers to try. These are mostly good for kids through elementary school, but tweens and teens may enjoy some of them too.
Spending time off the screen
Go outside. This sounds obvious, but spending time outdoors is something kids do less than they used to — and it can be really fun. If you have a yard, go out into it and play hide-and-seek or build a fort from snow or anything else that’s around. If you don’t have a yard, go to a local park or just go for a walk.
Go to the library. Do this early on in vacation, so that your child has lots of books to pass the time. Check out as many as they allow and you can carry.
Build a fort in the living room. Use blankets or sheets over chairs; if you have a small tent, set it up. Bring in pillows, sleeping bags, and flashlights; let the kids sleep in it at night. Let it stay up all vacation.
Build a city in the living room. Use blocks, Legos, boxes (or anything else), and add roads, cars, people, animals, trains, and other toys. Let it stay up all vacation, and make it bigger every day.
Getting creative off the screen
Get creative. Go to the craft store and stock up on inexpensive supplies. Buy things like poster board, huge pieces of paper (you could use those for your city, too, to make parks, roads, and parking lots), paints, and markers. You can make a paper mural, a comic book, a story, posters, or whatever catches your child’s imagination. If you know how to knit or sew, think about teaching your child or making a simple project together. Play music while you create.
Read out loud. There are so many books that are fun to read aloud. When my children were younger, we read the Harry Potter series out loud, as well as the Chronicles of Narnia and books by E.B. White and Roald Dahl. Act out the voices. Have some fun.
Have a puppet show. If you don’t have puppets, you can make some with socks — or you can hold up dolls or action figures and do the talking for them. You can make a makeshift stage by cutting out the back of a box and taping cloth (like a pillowcase) to fall over the front.
Get out the games. There are so many that work across the ages, like checkers, chess, Uno, Connect 4, Sorry, Twister, Clue, Scrabble, or Monopoly. We forget how much fun these can be.
Bake. You don’t have to get fancy — it’s fine to use mixes or pre-made cookie dough. There’s nothing better than baked goods straight from the oven, and adding frosting and decorations makes it even more fun. Turn on music and dance while things bake.
While parents or caregivers need to be involved with some of these activities (like the ones involving the oven, or reading out loud), kids can do many of them independently once you have it started. Which, really, is what children need: time to use their imagination and just play.
But you just may find that once you have things started, you want to play, too.
The post A low-tech school vacation: Keeping kids busy and happy without screens appeared first on Harvard Health Blog.
Wednesday, December 18, 2019
Medical News Today: Cancer drug shows promise in Parkinson's disease safety trial
Medical News Today: Why is it so difficult to make people change their minds?
Medical News Today: What is verbal abuse?
Medical News Today: What can cause an afternoon headache?
Medical News Today: What are the stages of the common cold?
Medical News Today: Eggs and cholesterol: Is industry funded research misleading?
Medical News Today: Does masturbation cause acne?
Medical News Today: Flu during pregnancy: What to know
Tuesday, December 17, 2019
Medical News Today: Having trouble sleeping: What to know
Medical News Today: What can you do to reduce fibroid pain?
Medical News Today: What is the best diet for mental health?
Medical News Today: Widowmaker heart attack: Everything you need to know
Medical News Today: When can a child sit in the front seat of a car?
Medical News Today: What does a radiologist do?
Medical News Today: Male scientists more likely to present findings positively
Medical News Today: FDA approve fish oil drug for cardiovascular disease
Medical News Today: Could hot chili peppers reduce mortality risk?
Medical News Today: E-cigarettes: How high is the risk of chronic lung disease?
Medical News Today: Weight gain during period: What to know
Medical News Today: How to reduce food waste
ACA open enrollment extended until 3 a.m. ET on Dec. 18
The original deadline was 11:59 p.m. on Sunday, Dec. 15. The last day is always the busiest, but many people trying to enroll via the website or by phone ran into delays and other issues. Despite the problems, the Centers for Medicare and Medicaid Services said in a statement that more than half a million people were able to enroll on Sunday. According to CMS, "people who already left their names and contact information with the call center on Sunday don’t need to come back and reapply because a representative will follow up with them later in the week," Ricardo Alonso-Zaldivar reports for The Associated Press.
Nonprofit organization Get America Covered urged the Trump administration to extend the sign-up period. The group was founded by former Obama administration officials to get the word out about ACA open enrollment after the Trump administration halved the sign-up period and slashed the budgets for advertising open enrollment and paying "navigators," or people who help others sign up for coverage, Alonso-Zaldivar reports.
Get America Covered co-founder Joshua Peck applauds the extension, but said he worries that they're not doing much to publicize or clarify the extension. The HealthCare.gov home page still says in large letters that 2020 open enrollment is over. A banner in much smaller letters at the top of the page notes that enrollment has been extended, which could confuse users, Sarah Gantz reports for The Philadelphia Inquirer.
"Senior lawmakers of both major parties are urging the administration to publicize the availability of a redo for seniors who got inaccurate or confusing results using the Medicare Plan Finder. A redesign of the Medicare site produced search results that didn’t automatically rank the prescription drug plan with the lowest total cost first," Alonso-Zaldivar reports.
Infertility: Grandparents in waiting
“Do you have grandchildren?” This seems like a simple question and one appropriate to ask women and men of a certain age. However, for those who are grandparents-in-waiting this question can bring layers of pain, fear, and challenge. These feelings are all the more powerful for grandparents-in-waiting who themselves experienced infertility years earlier, but they can wallop anyone whose child is struggling to have a child.
I’ll begin by defining “grandparents-in-waiting.” I use this to refer to people — usually in their 60s and 70s — who have adult children dealing with infertility or repeated pregnancy loss. Grandparents-in-waiting include those who already have grandchildren from their other adult children, and grandparents-in-waiting who have no grandchildren. There are also grandparents-in-waiting who face the dual challenge, or mixed blessing, of having a grandchild on the way through one daughter or son while another adult child grapples with infertility.
Feelings that may arise for grandparents-in-waiting
If you are a grandparent-in-waiting, here are a few of the feelings you might be experiencing or can anticipate.
Helplessness. There is a saying common among parents, “You are only as happy as your least happy child.” Whether one has zero grandchildren or 10, it is painful to see one’s child struggling to have a baby. You may be surprised to find yourself coping with your helplessness and lack of control by avoiding your friends. After all, many of them are grandparents, and being with them risks opening yourself up to news of new pregnancies or chatter about grandchildren.
Anger. By the time you reach your 60s or 70s, you’ve learned all too well that life is unfair. That said, it is hard to get away from the feeling that it is all so unfair. Pregnant women seem ubiquitous when your child is longing to be pregnant. If you are a veteran of your own infertility, you will recognize the nasty and harsh feelings that can arise toward pregnant women. If you had your own child or children with ease, these feelings can be unsettling. Grandparents-in-waiting need to know that angry, resentful feelings toward pregnancies — and even toward their friends’ grandchildren — don’t mean that they are turning into bad people.
Sadness. Having a child go through infertility, or suffer pregnancy loss, is a double sadness. You are sad for your child and you are sad for yourself, all the more so if you have no grandchildren. It is hard not to look around and feel that grandparenthood is a lottery. Some people have one child and wind up with four grandchildren. Others have four children and just one grandchild who lives thousands of miles away.
Rising to the challenge as a grandparent-in-waiting
Perhaps the biggest challenge for a grandparent-in-waiting is to deal with your own feelings without making things any more difficult for your child. Here are some guidelines for dealing with your daughter, daughter-in-law, or son during infertility.
- Let them control communication. Some adult children want to share their infertility struggles with their parents; some do not. If your child seeks privacy, respect that. Let them know that you are there if something changes and they want to talk.
If your child is open with you, talk with them about what helps and what does not. For example, they may want to fill you in on what is happening, but be upset if you offer advice or try to “help” more actively. An open discussion can help you avoid feeling like you are walking on eggshells. - Avoid any hint of blame. Regret is often the most painful part of infertility. Be aware that your child may blame herself or himself for “waiting too long,” “having other priorities,” or perhaps choosing the “wrong” doctor. Be there to listen but do all you can to avoid contributing to self-blame.
- Communicate acceptance. While grappling with infertility, people begin to think about other options such as adoption, egg donation, and surrogacy. If your child is beginning to consider “option B,” she or he will be sensitive to your reaction. It will mean a lot to your child to know that you will welcome and adore a grandchild regardless of how that child joins the family. That said, you need to be careful not to inadvertently communicate pessimism regarding current treatment. Your daughter or son could perceive your embrace of adoption or egg donation as evidence that you don’t think that their efforts on their own, or with IVF, will work.
- Be the parent. Your daughter may be super successful in her career, but right now she is your child and she needs you. Whether she communicates it or not, it means the world to her to know she can lean on you. By being the parent and doing your best parenting thing, you will let her know that you are there for her and that you are okay with your wait to be her child’s grandparent. She needs to feel that you are not suffering. Or perhaps more accurately, she needs to know that you can push your own pain firmly aside because your priority is to help diminish hers.
It is not easy to be a grandparent-in-waiting. Aging teaches all of us that life is short. Your wait for a grandchild is all the more difficult when you feel that you are losing precious time. There is no way to explain away or sugar-coat the loss of time. Still, I hope you are comforted to know that being able to be there for your child at this difficult time is a gift and a blessing.
The post Infertility: Grandparents in waiting appeared first on Harvard Health Blog.
Monday, December 16, 2019
Medical News Today: Are there symptoms for high blood pressure?
Medical News Today: Are some makeup ingredients toxic?
Medical News Today: Diabetes and anxiety: What is the link?
Medical News Today: What is a heavy metal detox?
Medical News Today: What does an internist do?
Medical News Today: How to safely dispose of medication
Medical News Today: How fish oil might reduce inflammation
Medical News Today: Same-sex sexual behavior in animals: Do we have it all wrong?
Medical News Today: Drumming makes your brain more efficient
DOACs now recommended over warfarin to prevent blood clots in people with atrial fibrillation
For decades, warfarin (Coumadin) was the standard anticoagulant medication used to prevent blood clots, which can lead to stroke, in people with atrial fibrillation (afib). Direct oral anticoagulants (DOACs), sometimes called novel oral anticoagulants (NOACs), are a new type of anticoagulant medication that came on the market in 2010.
In 2019, the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) updated their afib guidelines to strongly recommend using DOACs over warfarin in people with afib.
Warfarin is effective, but has downsides
Afib is a condition in which the upper chambers of the heart (the atria) quiver, and blood doesn’t flow well. This may lead to the formation of blood clots, which can travel to the brain and cause a stroke. Anticoagulants, which are also referred to as blood thinners even though they don’t actually thin the blood, make it harder for blood to clot and help keep existing clots from growing.
Warfarin was introduced into clinical practice for the prevention of clots associated with afib in the 1950s, and has proven to be a very effective therapy. Unfortunately, it requires close monitoring with blood tests to make certain that the blood does not clot too quickly or too slowly.
The ability to keep the blood thinned in the correct range can be very difficult because warfarin interacts with many foods and medications. In addition, up to 25% of the population is born with a genetic characteristic that makes it extraordinarily difficult to keep the blood thinned in the therapeutic range on warfarin.
DOACs more effective, less finicky than warfarin
Intensive efforts were underway for decades to develop alternatives to warfarin. This resulted in the FDA approval of four DOACs for clot prevention in atrial fibrillation, beginning in 2010: apixaban (Eliquis), dabigatran (Pradaxa), edoxaban (Savaysa), and rivaroxaban (Xarelto).
The use of DOACs compared with warfarin has been studied extensively, and we now have years of experience using these drugs. DOACs are remarkably free of side effects and do not require blood test monitoring. They have proven to be as effective as warfarin to prevent clot formation, and in some cases have proven to be slightly better than warfarin.
DOACs less likely to cause life-threatening bleeding
The major complication of taking any anticoagulation medication is bleeding. This risk is present with both warfarin and the DOACs. However, the risk of the most life-threatening form of bleeding — bleeding into the brain — has been shown to be roughly 50% less likely on the DOACs compared with warfarin.
One major concern I often hear from patients and physicians is that the blood-thinning effect of DOACs is irreversible. Fortunately, we now have antidotes for all of the DOACs. (The anticoagulant effects of warfarin are easily reversed with vitamin K.)
In addition, DOACs have a more rapid and predictable effect than we see with warfarin. DOACs thin the blood within a day; once stopped, the anticoagulation effect wears off quite rapidly, within 24 to 48 hours. It can take days to weeks for warfarin to thin the blood in the correct range, and at least three to five days before the blood is no longer thinned after stopping warfarin.
DOACs now seen as the better option for most people with afib
We are increasingly using DOACs as a first choice for anticoagulation in afib. We are also giving many patients the option to switch from warfarin to DOACs if they are already on warfarin. In general, this change can be made easily. The only patients with afib who should stay on warfarin rather than using a DOAC are those with a mechanical artificial heart valve.
There are some small differences between the different DOACs, but they are not major and can be discussed with your physician. For example, some DOACs may be better or worse for a patient depending on his or her kidney function.
The cost of these drugs is dropping, but is certainly more than warfarin. Increasingly, insurance companies cover their preferred DOAC, which makes using a non-preferred DOAC much more expensive. For most people, using the DOAC that is least expensive based on their insurance coverage is absolutely fine.
The post DOACs now recommended over warfarin to prevent blood clots in people with atrial fibrillation appeared first on Harvard Health Blog.
Sunday, December 15, 2019
Medical News Today: New birth control pill provides contraception for a month
Medical News Today: New food labeling system may reduce calorie intake
Four flu-related deaths have been reported in Kentucky; state health commissioner urges everyone to get vaccinated
Kentucky Health News
The Kentucky Department of Public Health has reported the first four influenza-related deaths of the 2019-2020 flu season, which runs through May.
“We extend our condolences to the families who have suffered losses during this flu season,” Dr. Angela Dearinger, commissioner of the agency, said in a news release. “These personal losses are a reminder for all of us that flu can be a serious illness, for young and old alike, and we strongly encourage people to protect themselves by getting a flu vaccination.”
Dearinger added that it is especially important for children and high-risk adults to get vaccinated, since they are at higher risk of complications and negative consequences, including death. She also encouraged anyone with flu to stay home and avoid contact with others.
It's also important to follow good hygiene practices to prevent the flu, like covering your cough and making sure you are washing your hands with soap and water for at least 20 seconds -- or the time it takes to sing "Happy Birthday" twice.
Health experts say it's also important to wash your hands after coughing, touching a door knob or handrail, and shaking hands. One regional health official has even advised Kentuckians to avoid hand shaking during the flu season, calling it "the worst thing you can do."
The federal Centers for Disease Control and Prevention recommends washing hands with soap and water whenever possible, and if not, to use a hand sanitizer with at least 60% alcohol.
 |
| Mortality and Morbidity Weekly Report map; click to enlarge |
During the week of Dec. 1-7, Kentucky saw 511 new confirmed cases of flu, with increases in 10 of the state's 17 health regions. Since Aug. 4, there have been 1,622 confirmed cases of flu in the state and all four of reported deaths were adults, according to the weekly influenza surveillance report.
Last season, the state had 17,665 confirmed cases and 196 flu-related deaths, including two children.
Flu symptoms include fever, headache, cough, sore throat, runny nose, sneezing and body aches. It is highly contagious. Persons who develop symptoms should contact their medical provider immediately to determine if they are a good candidate for treatment with an antiviral drug, which could shorten the course of the illness or reduce its severity.
The CDC recommends that everyone over six months of age get a flu shot, and it especially encourages people who may be at higher risk for complications or negative consequences to get one, including children 6 months to 5 years old and their caregivers; women who are or might be pregnant during flu season; people 50 and older and their caregivers; obese people; those with chronic health problems; residents of long-term care facilities, and health-care workers.
Vaccinations can be given any time during the flu season, but take about two weeks following the administration of the vaccine for the recipient to develop protection from the flu.
If you're looking for a place to get your flu shot, the CDC offers an interactive "flu vaccine finder" that allows you to type in your ZIP code to find nearby locations that offer shots. Local health departments offer the vaccine. Medicaid and Medicare and most private insurance providers cover flu vaccination at no cost to the patient as a preventive service.













